
by Charles R. Figley, Ph.D.
Purpose
The purpose of this webpage is to provide an overview of this important concept. Also, the purpose is to encourage collaboration toward building a sound theory and research base that will lead to effective programs for preventing and treating compassion fatigue encourage collaboration toward building a sound theory and research base that will lead to effective programs for preventing and treating compassion fatigue.
Introduction
In 1995 I collaborated to write Compassion Fatigue: Coping with secondary Traumatic stress Disorder in Those Who Treat the Traumatized (Figley, 1995). The book, Compassion Fatigue and Treating Compassion Fatigue are available from Amazon.com or from the publisher, Brunner/Mazel. Included in the book was a test for psychotherapists. You can complete it yourself on the web at one of two sites. The one here at my University and the other provided by ProQol self test . The test helps you determine the degree to which that were at risk of burnout and compassion fatigue. A new measure also includes a satisfaction scale in addition to burnout and compassion fatigue. This new measure is found here. For the latest version, visit Beth Stamm’s excellent web site, which has information on many measures. It is http://www.isu.edu/~bhstamm/. If you speak French, go here. If you are interested in working with animals, go here. If you work in disasters, go here.
The concept of Compassion Fatigue has been around only since 1992 when Joinson used the term in a nursing magazine. It fit the description of nurses who were worn down by the daily hospital emergencies. That same year Jeffrey Kottler (1992), in his book, Compassionate Therapy, emphasize the importance of compassion in dealing with extremely difficult and resistant patients. However, neither adequately define compassionate. Indeed, the term is not listed in the index of his book. It was mentioned only once in the final chapter on “Rules of Engagement.” Both authors, however, note how and why practitioners lose their compassion as a result of their work with the suffering.
The dictionary meaning of compassion is a “feeling of deep sympathy and sorrow for another who is stricken by suffering or misfortune, accompanied by a strong desire to alleviate the pain or remove its cause” (Webster, 1989, p. 229). Some would argue that it is wrong for a practitioner to have deep feelings of sympathy and sorrow for their client’s suffering. And certainly practitioners must understand their limitations in helping alleviate the pain suffered by their clients.
Yet, most systematic studies of the effectiveness of therapy point to the therapeutic alliance between client and clinician, the ability to empathize to understand and help clients (Figley & Nelson, 1989). If it is not present, it is highly unlikely that therapeutic change will take place. The most important ingredients in building a therapeutic alliance include the client liking and trusting her or his therapist. And these feelings are directly related to the degree to which the therapist utilizes and expresses empathy and compassion.
Recently my colleagues and I assembled TREATING COMPASSION FATIGUE. This book builds upon the 1995 volume. In the years since its publication, an impressive number of books, chapters, and articles were published. This book is an effort to further clarify the concept of compassion fatigue through theory, research, and treatment. The chapters are organized into sections consistent with these elements. This book will attempt to advance our knowledge and applications of compassion fatigue assessment, prevention, research, and treatment.
Contrasts Between Compassion Fatigue and Related Concepts
Compassion Fatigue is the latest in an evolving concept that is known in the field of Traumatology as Secondary traumatic stress. Most often this phenomenon is associated with the “cost of caring” (Figley, 1982) for others in emotional pain.
There are a number of terms that describe this phenomenon. It has been described as secondary victimization (Figley, 1982), secondary traumatic stress (Figley, 1983, 1985, 1989; Stamm, 1995; 1997), vicarious traumatization (McCann and Pearlman, 1989; Pearlman & Saakvitne, 1995), and secondary survivor (Remer and Elliott, 1988a; 1988b). A similar concept, “emotional contagion,” is defined as an affective process in which “an individual observing another person experiences emotional responses parallel to that person’s actual or anticipated emotions” (Miller, Stiff & Ellis, 1988, p.254). Also rape-related family crisis (Erickson, 1989; White & Rollins, 1981) and “proximity” effects on female partners of war veterans (Verbosky and Ryan, 1988) are related concepts. The generational effects of trauma (Danieli, 1985; McCubbin, Dahl, Lester, and Ross, 1977) and the need for family “detoxification” from war-related traumatic stress (Rosenheck and Thomson, 1986) have been noted. Finally, some view difficulties with client problems as one of simple countertransference and has been discussed within the context of PTSD treatment (Danieli, 1988; Herman, 1992; Maroda, 1991; Wilson & Lindy, 1994). However, the concept is encased in an elaborate theoretical context that is difficult to measure and traumatic issues from all others in the client-therapist transactions.
The American Psychiatric Association’s diagnostic disorders manual (DSM IV (APA, 1994) notes that Post-traumatic Stress Disorder (PTSD) is only possible when one is traumatized either directly (in harm’s way) or indirectly, as a parent. Both may experience trauma, though different social pathways. The latter pathway is called Secondary Traumatic Stress (COMPASSION FATIGUE). There are few reports of the incidence and prevalence of this type of stress reactions. However, based on secondary data and theory analysis, Burnout, Countertransference, worker dissatisfaction, and other related concepts may have masked this common problem (Figley, 1995). Vicarious traumatization, for example, refers to a transformation in the therapist’s (or other trauma worker’s) inner experience resulting from empathic engagement with clients’ trauma material. . .[and] vulnerable to the emotional and spiritual effects of vicarious traumatization. These effects are cumulative and permanent, and evident in both a therapist’s professional and personal life (Pearlman & Saakvitne, 1995, p. 151).
Compassion Fatigue is a more user friendly term for Secondary Traumatic Stress Disorder, which is nearly identical to PSTD, except it affects those emotionally affected by the trauma of another (usually a client or a family member). Indeed, my recent book on burnout in families (Figley, 1997) emphasizes the full extent of the negative impact of the family system. Burnout in Families is available from Amazon.com the publisher, CRC Press.
Compassion Fatigue, however, is related to the cognitive schema of the therapist (social and interpersonal perceptions or morale). Table 1 provide a useful contrast between the symptom criteria for PTSD and Compassion Fatigue. It is obvious that we can be traumatized by helping suffering people in harm’s way as well as being in harm’s way ourselves. Examples of Compassion Fatigue symptoms abound [See Chart 1 Symptoms]
We have suspected for some time that the same mechanism operating within families that account for this “spread” of the “virus” of PTSD within families is the same mechanism that accounts for vicarious traumatization experienced by professionals.
A recent book focuses on both the secondary traumatic stress and burnout found among modern families (Figley, 1997). Among the conclusions was that families both breed and destroy stress among its members and that PTSD spreads in the family like a virus unless families have ways to cope. This finding is consistent with others (Figley & McCubbin, 1983; Figley, 1989a; 1989b; Figley, 1995; Solomon, 1995). Thus, if stress is linked to a wide variety of medical and psychological ills (cf., Lazarus & Folkman, 1984), it is important to help families manage their stress-especially PTSD and other byproducts of catastrophe. Compassion fatigue is one form of burnout. Family burnout is its interpersonal equivalent (Figley, 1997).
A recent study (Barnes, 1997) of emergency medical personnel, for example, found that parents are traumatized out of caring for their injured child. The consensus among these experts: Families need more attention to both heal themselves and the member most physically injured. Indeed, the trend in the 1990s has been toward greater support for the American family to cure many social ills. In a recent interview, Figley (Peeples, 2000), discusses this and other studies of family burnout and the role of family specialists in helping families cope.
Extent of the Problem of Compassion Fatigue
This volume reports on five research projects that investigated the incidence and prevalence of compassion fatigue among professionals working with the suffering. The picture that emerges is clear: Those who work with the suffering suffer themselves because of the work. A recent study is illustrative.
In a doctoral dissertation, Lee (1995), based on the data analysis of 132 Marriage and Family Therapists (MFT), drawn from those listed in their national association’s directory, found a statistically significant relationship (r=.20) between and Compassion Fatigue scores and caseload dissatisfaction. The results indicate that CF was significantly correlated with Compassion Fatigue. The results also indicated that MFT professionals experienced Compassion Fatigue that was higher than medical students did but lower than PTSD stress clients did. MFT professionals in the sample had an average of 63% of their client load was traumatized. However, MFT professionals, as a group, are experiencing only a moderate level of Compassion Fatigue, as measured by the IES.
The study predicted and found a strong relationship between Compassion Fatigue and various cognitions associated with general morale in one’s personal and professional life (Cognitive Schema). The usual limitations of survey-based studies requiring retrospective, self analysis apply to this study (Borg & Gail, 1983; Brigham, 1986; Fincham & Bradbury, 1987).
The results show that a measure of Cognitive Schemas was significantly correlated (r = .34) with a measure of Compassion Fatigue. These results support the relationship and, perhaps, overlap, between these two variables. Future research should use additional measures of Compassion Fatigue (e.g., Self-Test for Psychotherapists in Figley, 1995) and additional measures of Cognitive Schemas (Stamm, 1996). Further speculations about the implications of these findings are risky until other studies confirm the relationship. However, there is growing, indirect evidence that perceptions about self worth (personally and professionally) and the value of family, friends, community, and other social resources are closely related to general morale.
Another recent report of an unpublished study (Pelkowitz, 1997) notes that nurses working in a Trauma Unit in South Africa with prisoners were especially vulnerable to compassion fatigue. Equally useful, Pelkowitz offered a useful table on the impact of compassion fatigue. Chart 2 drew from her original conceptualization and many of the symptoms.
In an exhaustive review of the professional literature, Beaton and Murphy (1995) assert that emergency or first responders and crisis workers absorb the traumatic stress of those they help. By doing so, they are at risk for experiencing compassion fatigue. Among the negative consequences that are often not linked to their work include substance abuse and relationship conflicts. This is consistent with the finding of McCammon and Jackson (1995) who reviewed the emergency medical professionals.
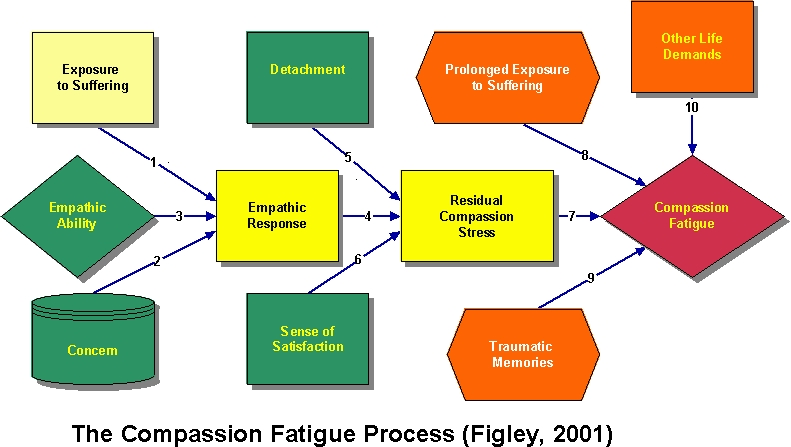
One central question in future studies should be: Who is most vulnerable to Compassion Fatigue in what type of work setting, under what types of conditions, and, once developed, how can it be treated and return the worker back to good morale. These questions are addressed in Figley, 1995. One line of research involves investigating the utility of a Model of Compassion Stress/Fatigue.
Moreover, since research suggests that there is a significant overlap in effectiveness of various PTSD treatment methods found useful for clients suffering from PTSD and the methods found useful for professionals suffering from Compassion Fatigue. This is the basic thesis of this volume.
In the years since Compassion Fatigue: Coping with Secondary Traumatic stress Disorder in Those Who Treat the Traumatized (Figley, 1995), an impressive number of books, chapters, and articles were published. Research, assessment, and program evaluation must continue. However, what is critically needed now is preventing and treating compassion fatigue. Visit the Academy of Traumatology web site for information on training opportunities for certification in compassion fatigue prevention.
References
American Psychiatric Association (1994). Diagnostic and statistical Manual of Mental Disorders (4th Edition). Washington, D C: Author.
Barnes, M. F (1997). Understanding the secondary traumatic stress of parents. In C. R. Figley (Ed). Burnout in Families: The Systemic Costs of Caring, pp., 75-90. Boca Raton: CRC Press.
Burgee, S. K. (1983). Rape: Individual and family reactions. In C. R. Figley and H. I. McCubbin (eds.). Stress and the Family, Volume II: Coping with Catastrophe. New York: Brunner/Mazel, 103-119.
Catherall, D. R. (1997). Treating traumatized families. In C. R. Figley (Ed). Burnout in Families: The Systemic Costs of Caring, pp., 187-216. Boca Raton: CRC Press.
Beaton, R. D. and Murphy, S. A. (1995). Working with people in crisis: Research implications. In C. R. Figley (Ed.), Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized, 51-81. NY: Brunner/Mazel.
Danieli, Y. (1985). The treatment ad prevention of long-term effects and intergenerational transmission of victimization: A lesson from Holocaust survivors and their children. In C. R. Figley (Ed.), Trauma and its wake, pp 295-313. NY: Brunner/Mazel.
Danieli, Y. (1988). Treating survivor and children of survivors of the Nazi Holocaust. In F. Ochberg (Ed.), Post-traumatic Therapy and Victims of Violence, pp. 278-294. NY: Brunner/Mazel.
Derogatis, L. (1994). SCL-90-R Symptom Checklist-90-R. Administration, Coding, and Procedures Manual. National Computer Systems, Inc., Minneapolis, MH.
Erickson, C. A. (1989). Rape and the family. In C. R. Figley (1989). Treating stress in families, 257-290. NY: Brunner/Mazel.
Feinauer, L. (1982). Rape: A family crisis. American Journal of Family Therapy, 10:4, 35-39.
Figley, C. (1982). Traumatization and comfort: Close relationships may be hazardous to your health. Keynote presentation at the Conference, Families and close relationships: Individuals in social interaction, Texas Tech University, Lubbock, Texas, February.
Figley, C. R. (1983). Catastrophes: A overview of family reactions. In C. R. Figley and H. I. McCubbin (Eds.), Stress and the Family: Volume II: Coping with Catastrophe. New York: Brunner/Mazel, 3-20.
Figley, C. R. (1985). The family as victim: Mental health implications. Psychiatry, 6, 283-291.
Figley, C. R. (1986). Post-traumatic stress: The role of the family and social support systems. In C. R. Figley (Ed.), Trauma and Its Wake: Volume 2. Post-Traumatic Stress Disorder: Theory, Research, and Treatment. New York: Brunner/Mazel.
Figley, C. R. (1986). Traumatic stress: The role of the family and social support system. In C. R. Figley (ed.), Trauma and Its Wake, Volume II: The Study and Treatment of Post-Traumatic Stress Disorder. New York: Brunner/Mazel, 39-54.
Figley, C. R. (1989a). Helping Traumatized Families. San Francisco: Jossey-Bass.
Figley, C. R. (Ed.) (1989b). Treating Stress in Families. NY: Brunner/Mazel.
Figley, C. R. (1992b). Secondary traumatic stress and disorder: Theory, research, and treatment. Paper presented at the First World Meeting of the International Society for Traumatic Stress Studies, Amsterdam, June.
Figley, C. R. (1993). Compassion stress: Toward its measurement and management. Family Therapy News (January).
Figley, C. R. (Ed.) (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. NY: Brunner/Mazel.
Figley, C. R. (Ed.) (1997). Burnout in Families: The Systemic Costs of Caring. New York: CRC Press.
Figley, C. R. & Kleber, R. (1995). Beyond the “victim”: Secondary traumatic stress. In R. Kleber, C. R. Figley, and B. P. R. Gersons (Eds.), Beyond trauma: Cultural and societal dynamics (pp.75-09. NY: Plenum.
Figley, C. R. and McCubbin, H. I. (Eds.)(1983). Stress and the Family, Volume II: Coping with Catastrophe. New York: Brunner/Mazel.
Figley, C. R. & Nelson, T. (1989). Basic family therapy skills, I: Conceptualization and initial findings. JOURNAL OF MARITAL AND FAMILY THERAPY, 15:4, 211-130.
Figley, C. R. (2001). Renewing Spirits: Lessons From Thirty Years of Trauma Work, Invited keynote address to the William Wendt Center for Loss and Health Conference on Illness, Grief & Trauma, Washington, DC, October 6.
Frederick, C.J. (1985). Children traumatized by catastrophic situations. In S. Eth and R.S. Pynoos (Eds.), Post-traumatic stress disorders in children (pp. 71-100). Washington D.C: American Psychiatric Press, Inc.
Frederick, C.J. (1987). Psychic Trauma in Victims of Crime and Terrorism. In G.R. Vandenbos and B.K. Bryant (Eds.), Cataclysms, Crises and Catastrophes: Psychology in Action Master Lecture Series. Washington, D.C.: American Psychological Association.
Herman, J. L. (1992). Trauma and recovery: The aftermath of violence–from domestic abuse to political terror. NY: Basic Books.
Hilfiker, D. (1985). Healing the Wounds: A Physician Looks at His Work. NY: Pantheon Books.
Kottler, J. A. (1992). Compassionate Therapy: Working with Difficult Clients. San Francisco: Jossey-Bass.
Joinson, C. (1992). Coping with compassion fatigue. Nursing, 22:4, 116-122.
Maslach, C. and Jackson, S. E. (1981). The measurement of burnout. Journal of Occupational Behavior, 2, 99-113.
Maslach, C. (1976). Burn-out. Human Behavior, 5 (9), 16-22.
McCammon, S. L. and Allison, E. J. (1995). Debriefing and treating emergency workers. In C. R. Figley (Ed.), Compassion fatigue: Coping with secondary traumatic stress disorders in those who treat the traumatized, 115-130.
McCann, I. L. and Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3:2, 131-149.
Miller, K. I., Stiff, J. B., & Ellis, B. H. (1988). Communication and empathy as precursors to burnout among human service workers. Communication Monographs, 55(9), 336-341.
McCubbin, H. I., Dahl, B. B., Lester, G., and Ross, B. (1977). The returned prisoner of war and his children: Evidence for the origin of second generational effects of captivity. International Journal of Sociology of the Family, 7, 25-36.
Pearlman, L A. & Saakvitne, K. W. (1995). Treating therapists with vicarious traumatization and secondary traumatic stress disorders. In C. R. Figley (Ed.), Compassion fatigue: Coping with secondary traumatic stress disorders in those who treat the traumatized, 150-177. NY: Brunner/Mazel.
Remer, R. & Elliot, J. (1988). Characteristics of secondary victims of sexual assault. International Journal of Family Psychiatry, 9:4, 373-387.
Rosenheck, R. and Thomson, J. (1986). ‘Detoxification’ of Vietnam war trauma: a combined family-individual approach. Family Process, 25:4, 559-570.
Stamm, B.H. (Ed.) (1995). Secondary traumatic stress: Self-care issues for clinicians, researchers and educators. Lutherville, MD: Sidran Press.
Stamm, B.H. (1997). Work-related Secondary Traumatic Stress. PTSD Research Quarterly, (8) 2, Spring. [Available on-line [http://www.dartmouth.edu/dms/ptsd/RQ_Spring_1997.html.]
Stamm, B.H. & Pearce, F.W. (1995). Creating virtual community: Telemedicine applications for self-care. In B.H. Stamm. (Ed.), Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers and Educators. Lutherville, MD: Sidran Press.
Verbosky, S. J. and Ryan, D. A. (1988) studied the female partners of Vietnam veterans: Stress by proximity. Issues in Mental Health Nursing. 9:1, 95-104.
Webster’s Encyclopedic Unabridged Dictionary of the English Language. NY: Gramercy Books.
White, P. N. & Rollins, J. C. (1981). Rape: A family crisis. Family Relations, 30 (1), 103-109.
Wilson, J. P. and Lindy, J. D. (1994). Countertransference in the Treatment of PTSD. NY: Guilford
